Achilles Tendon Injuries: Prevention, Rehab, and Recovery
Introduction
Did you know the Achilles tendon is the strongest tendon in the human body? Despite its strength, it's not indestructible. As a physical therapist, I frequently treat patients with a wide range of Achilles tendon injuries from mild, nagging tendinopathy to full ruptures. These injuries don’t just affect weekend warriors. Professional athletes are also susceptible, particularly in sports that demand quick and explosive movements.
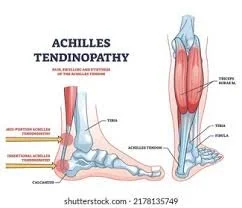
The Achilles tendon connects the calf muscles, specifically the gastrocnemius and soleus, to the heel bone (calcaneus). It plays a vital role in walking, running, jumping, and pushing off the foot. Because of its constant involvement in movement, the Achilles tendon is especially prone to overuse and strain.
In both athletic and general populations, these injuries can be painful, frustrating, and slow to heal. In athletes, they can even be career ending. The good news is with proper education, preventative strategies, and structured rehabilitation, many Achilles injuries can be avoided or successfully managed.
The Root Causes of Achilles Tendon Injuries
Achilles tendon injuries rarely occur suddenly. More often, they develop gradually due to overuse or excessive loading without adequate recovery. This is why we commonly see them in individuals who rapidly increase their training intensity, such as recreational athletes, weekend warriors, or those who are overtraining without rest.
While overuse is the primary culprit, several contributing factors can increase the risk of injury:
Limited ankle mobility, especially restricted dorsiflexion
Reduced calf muscle endurance
Weakness in the posterior chain (glutes and hamstrings)
Calf tightness or poor flexibility
Improper or unsupportive footwear
Biomechanical abnormalities like overpronation (flat feet)
Addressing these issues through thorough assessment, corrective exercise, and proper load management is key to both preventing and rehabilitating Achilles injuries.
Recognizing the Warning Signs
Our bodies have built-in warning systems, and the Achilles tendon is no exception. Unfortunately, many people ignore early symptoms, pushing through pain until the condition worsens. Recognizing these signs early is essential for avoiding long term complications.
Common symptoms of Achilles tendon issues include:
Morning stiffness or discomfort with the first few steps
Tightness in the calves
Swelling or thickening along the tendon
Pain during activities that involve pushing off the toes (e.g., stairs, hills, running, jumping)
If you’re experiencing any of these symptoms, don’t brush them off. Early intervention can significantly reduce recovery time and prevent the condition from progressing.
How to Prevent Achilles Injuries
One of the most effective ways to prevent Achilles injuries is through progressive strengthening of the calf muscles. Despite increased awareness around fitness and strength training, the calves are often overlooked—even though they play a critical role in walking, running, jumping, and standing.
The calf complex consists of two main muscles:
Gastrocnemius – more active when the knee is extended
Soleus – more active when the knee is bent
Both muscles help absorb and produce force, which reduces strain on the Achilles tendon.
A common misconception is that tight calves only need stretching. While flexibility is important, a more effective strategy includes:
Ankle mobility drills to improve joint range
Functional (weight bearing) calf stretching
Targeted strength training for the calf complex
Gradual progression of training volume and intensity
The Achilles tendon is designed to withstand high levels of stress, but if not properly conditioned, it becomes vulnerable to strain or rupture. In the early stages of tendon irritation, isometric holds like sustained heel raises can reduce pain and begin the loading process. As symptoms improve, eccentric exercises, which lengthen the tendon under tension, help build strength and resilience where the tendon is most likely to fail during explosive movement.
Training habits also play a key role in prevention:
Avoid sudden spikes in training volume
Follow the 10 percent rule: increase total volume by no more than 10 percent per week
Add variety to workouts by changing movements, intensity, and direction of force
As strength and tolerance improve, more advanced movements such as jumping, hopping, and change of direction drills may be introduced to further enhance tendon durability. These should only be added once a solid foundation of mobility and strength has been established.
Knowing When You're Ready to Return
Tendon injuries can be deceptive. Once pain subsides during daily activities, it's easy to assume you're fully recovered. But returning too soon to the same sport or movement pattern can lead to reinjury.
A structured, progressive rehab plan is critical. Once pain resolves and single leg eccentric exercises are well tolerated, the next phase should include plyometric drills, jumping, hopping, and change of direction movements, to ensure the tendon can handle higher level demands.
The goal is to bridge the gap between isolated rehab exercises and real world performance.
Remember: rehab is rarely linear. Setbacks happen. Regular reassessment allows for tailored adjustments in volume, intensity, and complexity, keeping recovery on track.
When to Seek Help
Struggling to manage an Achilles injury on your own? If you've stopped doing the activities you love, don’t wait any longer. The longer you delay care, the longer the recovery process can take.
Early intervention leads to better outcomes and a faster return to doing what you enjoy. Achilles tendon injuries may be frustrating, but they are treatable.
Get evaluated by one of our movement specialists today and let’s make sure you’re not staying sidelined any longer than necessary.